Gallstones and Gallbladder Surgery
Please click the questions below to reveal the answer
The gallbladder is an organ situated underneath the liver. It is a storage reservoir for bile, which is required for fat digestion. Bile is a mixture of cholesterol, bilirubin, bile salts and lecithin. After eating fatty food, the body produces a hormone called Cholecystokinin which in turn promotes the gallbladder to squeeze additional bile into the gut via the bile duct. You can live without your gallbladder as bile can also directly enter the gut from the liver through the bile duct.
You don't need a gallbladder in order to digest food properly. If your gallbladder is removed, bile will flow directly from your liver through the bile duct and into the small intestine.
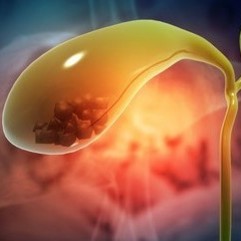
Gallstones are stone-like objects made of cholesterol or bilirubin. They can develop in the gallbladder or bile ducts. They can vary in size from sediment to very large stones.
Gallstones are found in approximately 10–20% of the global adult population, and >20% of people with gallstones will develop symptoms in their lifetime.
Gallstones are thought to develop because of an imbalance in the chemical make-up of bile inside the gallbladder.
Cholesterol Stones (90%) - Your bile contains too much cholesterol. Normally, your bile contains enough chemicals to dissolve the cholesterol excreted by your liver. But if your liver excretes more cholesterol than your bile can dissolve, the excess cholesterol may form into crystals and eventually into stones.
Pigment Stones (10%)- Your bile contains too much bilirubin. Bilirubin is a chemical that's produced when your body breaks down red blood cells. Certain conditions cause your liver to make too much bilirubin, including liver cirrhosis, biliary tract infections and certain blood disorders.
Genetics – A study in 43,141 Swedish twin pairs with gallstone disease indicated that approximately 25% of the risk of gallstone disease is determined by genetics.
Metabolic Syndrome: obesity, non-alcoholic fatty liver disease, insulin resistance and Diabetes Mellites, physical inactivity.
Pregnancy - Interestingly, in up to 60% of women, gallstones can disappear post-partum due to decreased levels of Oestrogen.
Medications - Oestrogens, Progesterone, Fibrates, Calcineurin Inhibitors and Octreotide.
Dietary factors - High-calorie intake, high-carbohydrate intake, high-glycaemic load, low-fibre intake, high-haem iron intake.
Rapid weight loss (that is, >1.5 kg per week by a very-low-calorie diet or after bariatric surgery caused gallstones in 30% of patients)
Prolonged Total Parenteral Nutrition (TPN)
Spinal cord injury
Gastrectomy (due to vagal nerve division)
Factors increasing enterohepatic bilirubin cycling - Liver cirrhosis; Crohn’s disease, Right Hemicolectomy
Biliary colic - if a gallstone becomes trapped at the neck of the gallbladder, it can trigger a sudden, intense pain under your rib cage lasting between 1 and 5 hours. It is usually triggered by the ingestion of fatty foods.
Cholecystitis (Inflammation of the gallbladder) - A gallstone that becomes lodged in the neck of the gallbladder can also cause inflammation of the gallbladder. Cholecystitis can cause severe pain and fever lasting for several days and may require antibiotics or gallbladder removal (cholecystectomy).
Obstructive Jaundice (blockage of the common bile duct) - gallstones can block the tubes (ducts) through which bile flows from your gallbladder or liver to your small intestine. Severe pain, jaundice and bile duct infection (cholangitis) can result.
Pancreatitis - A gallstone can cause a blockage in the pancreatic duct, which can lead to inflammation of the pancreas (pancreatitis). Pancreatitis causes intense, constant abdominal pain and vomiting and usually requires hospitalization.
Overall, 1–4% of individuals with previously diagnosed asymptomatic gallbladder stones develop symptoms every year. Of those who present with symptoms, biliary colic is often the main symptom. Based on a balance of benefits and harms, there is currently no evidence to support routine cholecystectomy in patients with asymptomatic gallbladder stones, except in cases of suspected gallbladder cancer such as a porcelain gallbladder or polyps greater than 1cm.
Suspected cancer
Biliary dyskinesia – Functional abnormality of the gallbladder
Acalculous cholecystitis with evidence of gangrene or perforation
Gallstones may have been present before pregnancy or can develop during pregnancy. Decision to proceed to cholecystectomy depends on the stage of pregnancy and the disease severity. In most women, supportive management of uncomplicated gallstones can delay cholecystectomy until the post-partum period. Cholecystectomy provides definitive management of problematic gallstones, but the stage of pregnancy must be considered. The second trimester is believed to be the optimal stage of pregnancy for cholecystectomy, with the lowest risk for foetal morbidity. Interestingly, in up to 60% of women, gallstones can disappear postpartum due to decreased levels of Oestrogen.
Make an appointment with your doctor if you have any signs or symptoms that worry you. Seek immediate care if you develop signs and symptoms of a serious gallstone complications including intense abdominal pain, jaundice and fever.
The most effective treatment for symptomatic gallstones found in the gallbladder is to remove the gallbladder surgically. Removal of the gallbladder is called a cholecystectomy. In the majority of cases this surgery can be performed as a keyhole operation (laparoscopic cholecystectomy).
Common bile duct stones either occur by migration from the gallbladder or (less frequently) develop in the bile duct. Coexistent bile duct stones are found in 3–16% of patients with symptomatic gallbladder stones, often with subsequent spontaneous passage to the duodenum.
If gallstones are present in the bile duct in addition to the gallbladder on pre-operative imaging, then the procedure of choice is to remove the gallstones from the bile duct with Endoscopic Retrograde Cholangiopancreatography (ERCP) prior to the gallbladder removal. Other options include removing the bile duct stones at the time of laparoscopic cholecystectomy, however cases need to be carefully selected.
Currently there is no evidence that medical dissolution treatment with Ursodeoxycholic Acid or Extracorporeal Shockwave Lithotripsy is effective in the treatment of gallbladder stones, as the rates of cure (that is, the permanent clearance of gallstones) are low and the recurrence rates of gallstones are high.
Laparoscopic Cholecystectomy is considered a relatively safe procedure but like all operations there is a risk of complications. General risks of laparoscopy are small but include infection, bleeding, damage to intra-abdominal organs, venous thrombo-embolism, myocardial infarction, stroke and incisional hernia. Risks specific to cholecystectomy include a 1 in 500 risk of bile duct injury. If this happens it needs fixing and nearly always involves a bigger operation and a longer recovery. Bile leaks can also occur and may require drainage +/- an Endoscopic Retrograde Cholangiopancreatography (ERCP) and stent insertion. Stones can also be retained in the bile duct and usually pass of their own accord but sometimes cause pain and jaundice and need an ERCP for removal in the post-operative setting. Approximately 5% of patients may experience diarrhoea postoperatively. In the majority of patients this settles down.
Removal of the gallbladder can alter bile acid metabolism. In particular, it raises the faecal concentration of deoxycholic acid, this bile acid being an agent that sensitises the rectum and can cause an urge to defecate. In most cases, the diarrhoea stops soon after the surgery but in approximately 5% of patients it can persist. A SeHCAT study can be used to diagnose Bile Acid Diarrhoea (BAD) secondary to cholecystectomy. Positive response to the medication, Cholestyramine, in these patients is approximately 80%.
It will take approximately 2 weeks to recover from Laparoscopic Cholecystectomy.
Daily activity – Mobilise as soon as possible after surgery and try to keep active.
Washing – You are free to shower any time after the operation as you will have a waterproof glue dressing on the skin. The glue can be peeled off on day 7. Avoid bathing, jacuzzi or swimming for the first 2 weeks after the operation.
Driving – Always check with your individual insurance company but most would advise abstaining for 1 to 2 weeks depending on whether you have stopped any strong pain killers such as Codeine and or can do an emergency stop without pain.
Exercise – safe to return to cardiovascular exercise at 4 weeks and lifting weights with caution at 6 weeks.






